|
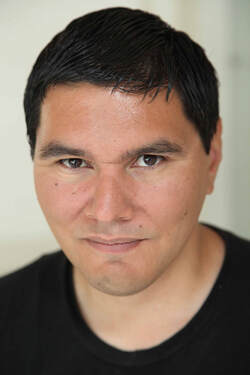
This week on No Restraints with Rudy Caseres my guest is Krista MacKinnon. Krista has specialized in mental health recovery education, curriculum development, group facilitation and community organizing since 2003. She created Families Healing Together, one of the first ever online family mental health recovery education programs, which has been utilized by over 1000 families across five continents, and has been contracted with agencies in Canada, Australia and the US. Krista also works in Community Outreach and Family Support for Muir Wood Adolescent and Family Services. You can learn more about Krista's work at familieshealingtogether.com and muirwoodteen.com.
See you again next week for an all-new No Restraints with Rudy Caseres. Wednesdays 12pm PT/3pm ET. Watch live at Facebook.com/RudyCaseres and, of course, watch all past episodes at NoRestraints.net. Why? Because it's for your own good.
TRANSCRIPT:
Rudy: Hey everyone, welcome to a brand new episode of No Restraints. This is a little weird because today, Wednesday, July 3rd, the great Facebook Outage of - I think it's the second one, but whatever of 2019 and so instead of just rescheduling or calling and off altogether, here I am, what? Krista McKinnon, we're not going to do it live, but we're going to post this when Facebook is letting us again when it's got his shit together and we're going to have a quality conversation. You and I, Krista, and this is still No Restraints. This is still episode 49. It's a little different. So thank you for working with me, Krista. Without further ado, who is Krista McKinnon? Krista: I am a person who's recovered from a childhood diagnosis of bipolar disorder. I am a person that believes very deeply in connection, um, and finding ways for strange relationships to be strengthened. I've done, I've worked for a few different organizations. I've done speaking and presenting across Australia, United States and Canada. And yeah, basically I'm a person who spends a lot of my time caring about and thinking about families in mental health and addiction recovery. Rudy: Now a word that you used and I hear a lot throughout your work, especially with families healing together is "recovery." Which can mean a lot of different things to a lot of different people and a lot of different communities. Very controversial. Some people hate it, some people will love it and everything in between. So your definition, Krista Mackinnon, what is recovery? Krista: Well, it's so fascinating because I've worked in mental health specifically for most of my adult life and only in the past year have I started to work in addictions. And of course addictions and mental health are absolutely interrelated. Everyone knows this, but they do tend to operate in silos. I mean there are mental health services and their recovery services and, and peer supports in mental health services and in recovery services, uh, for addiction are quite different. I mean, addiction has a whole AA community, which is, you know, has a deep history and it's all over and is flourishing. And, um, you know, in mental health, mental health recovery is relatively new. Even the concept of it is relatively new, especially compared to what's happening, organizing around AA and things like that. So you asked my personal definition of recovery. So I identify as a person who's in recovery in that I spend my, a lot of my life, a lot of my energy in my heart in learning to be free. So I was born free and then life happened. Trauma happened. Just sexual abuse, a history of diagnosis, recovering from that diagnosis, marriage, divorce, you know, immigration to countries, poverty, not poverty anymore. Poverty again, I mean, just life. And so how I personally identify with the word recovery is I'm a person in recovery trying to recover my freedom, which is my birthright to be a free being. When I talk about recovery in the work I do with families. I'm talking about their family recovery. So in spite of whatever whatever chaotic scenarios are happening in the family due to a mental illness due to mental health issues there that their family can recover a semblance of connectivity, love, freedom, joy as a family. So I needed it. Like some countries will define, you know, the definition of mental health recovery as being like living well in the presence or absence of illness and like, you know, there are definitions like that. So there are a million different ways you can define mental health recovery. But yeah, that's my personal definition. And when I talk about family mental health recovery, what I'm actually talking about is taking everything that we've learned about mental health recovery and mental health recovery and systems planning, taking all of that wisdom and leveraging it to educating families on how they can implement recovery in their family life. Rudy: Now I've heard people in the Mad Pride, psychiatric survivor movement saying they don't like the word recovery because what are they recovering from? They're fine. It's the people that are putting these diagnoses on them and saying that you need to recover what say you to that. Krista: Yeah, well, I mean, everybody has to recover from trauma all the time, even if it's just the trauma of, you know, even if it's a micro trauma. I mean, we all have traumas that happened in our lives all the time that we need to recover from. But recovery, you know, as a term is, is an unwieldy because there's recovery as a systems approach to managing the mental health system. Then there's individualized recovery. Then there's recovery as a practice like psychosocial rehabilitation recovery. So, I mean, it's like, it's very unwieldy. You know, if somebody's a psychiatric survivor, as you said, would say, "I hate the word recovery. I don't have to recover from anything. It's all these people telling me that I'm sick when I'm not sick, or something to that effect." Like, you still have to recover from the fact that you live in a culture that is, I'm treating you in such a way that doesn't align with your version of reality. Right? I mean, that's, that's intense. How do you live in, you know, in a world where everybody's saying one thing about you that you don't believe to be true, that you need to recover from that experience. So there's, you know, there are many different ways of taking that word and applying it. Rudy: Now let's take the diagnosis that you had - bipolar disorder. Talk about how you got that, how you viewed it thin and how you view it now. Krista: So I was 16 when I received my diagnosis, I was forced into treatment and I had an inpatient stay for five weeks. I was kind of just hanging with the wrong crowd, I guess you could say. I mean, I was doing drugs. I was doing acid and smoking cannabis most specifically before I had my, what they called Manic episode that got me hospitalized. So what happened at the time was I was forced, treated for something they called bipolar disorder. I was told to be on, you know, that I had a lifelong brain disease that I would need to be on medication for the rest of my life. My parents were taught to believe that about me as well. And they were also taught to be sort of the gatekeepers up too much. Not The gatekeepers, but like guards in a way. They were letting, you know, they were trained by the hospital to, you know, make sure she takes her medication. It's absolutely dangerous. If she goes off it, she'll have another psychotic episode. She needs to be on this because she has this brain disease called bipolar sore. I never fully bought into that belief. So, you know, when you're 16, those are like formative years. You're figuring out who you are. I'm almost 40 and I'm still figuring out who I am and in terms of how I relate to the diagnosis now versus how I related to it, then I still don't buy it. I still don't swallow it. Hook, line and sinker. I think that people are diagnosed with what the medical community considers a lifelong brain disease and mental illness at young ages way too often. And that that's dangerous because when you're diagnosed with something like that, even someone like me who's like, [inaudible], I'm not taking that. I don't believe that. It doesn't go away. It's like you, you've had this diagnosis and whether or not you believe it and whether or not you live well for the rest of your life, whether or not you're on medication or not, you have that. It's just part of you. You always are wondering like, is this thing, you know? So I don't know. I mean, how do I relate to it now? I don't access psychiatric supports for my emotional states. I have spent a lot of my life studying wellness practices and enhancing my own personal medicine strategies. And I live really well and I love life. And I'm grateful for my life. So I don't feel like I exist in the world as an ill person. Rudy: Let's talk about mania. Is that something that you experienced in those younger years or is it something you still deal with now? Krista: I haven't dealt with it lately. I dealt with it in my young years. That's why I had a manic episode, what they called a manic episode. So, which is what had me hospitalized. And I didn't officially, I was never hospitalized again, so I was able to sort of anytime I had experiences that could have been identified as mania I managed them in such a way that I didn't end up in the hospital again or - but yeah. I think I've had times in my life where I was tapped into a different kind of frequency that is not ordinary. Rudy: So if you are not, if you were going to use a word other than mania to describe your experience, what would you use? Krista: I mean I don't even mind personally. I don't mind the term "mania". It happens to be a medical term. But I don't mind it because I think it can accurately describe, I mean for me it's more of like sped up. Like I prefer the term "I'm sped up right now." Or "high." Rudy: So if you were to get really, really sped up or high right now, how would you manage that? Krista: Well, this is where I have personal practices. Like this is why I identify as being partially still as being in recovery because I have practices that I have to kick up, you know, if I noticed myself, I'm straying from center, then I have to kick up on my practices and my prac - my personal practices are breath work and yoga. And it's a particular kind of breath work that I do that's called rebirthing breath work, founded in 2012 and has been, I'm so grateful to it because it's really helped me to live from my inner compass in a way that I didn't even know I had an inner compass, I think at times. So, yeah, so I have personal practices and that like, you know, Patricia Deegan, Dr Patricia Deegan calls them personal medicine, right? So my personal medicine is work. And so if I'm feeling, if I know, if I know my thoughts are going in it to a place that are, I'm not going to help me in my life, then I kick up my practices. Rudy: So do you see mania as something to avoid or something necessarily bad? Krista: No. Nope. It depends how that, how the mania manifests. This is like - the Icarus Project has, they say, you know, navigating the space between brilliance and madness. So, and I really identify with that and I've got a lot of support through the way that they've explored understanding madness because my, my mania, uh, you know, is what it has helped me to birth projects has helped me, you know, not to Romanticize it, but you know, my positive like manifestations of mania I have been, I get great ideas, I write more, it gives me courage to make really bold decisions that from an outside perspective often look like I'm not thinking straight, but they, but some of those bold decisions that really worked out for me. And I think that there's a certain degree of crazy that I'm blessed with that sort of allows me to do things that not everybody would do or that allows me to not feel my comfort zone in such a painful way. So I'm able to step out of it. And those are like the gifts in terms of navigating the gifts of, you know, brilliance and madness. Like there's some gifts to it. And another thing is once you've been diagnosed as somebody who is mentally ill or has a mental illness, um, which is not language I personally use, but that's what the culture gave me that language to identify myself. Um, and once, once you've been given that there's, there's a way in which I stopped caring what people thought about me, it's like, okay, well people think I'm crazy anyway. So it's kind of helped me to shed a skin around, just worry about what other people think in a way. Rudy: Yeah, you used that word romanticizing. And I think that's something we personally get scared of when talking about the positives of mania, bipolar, because I've even been told that I'm manic for saying that or I'm delusional or just my illness talking. And it's a tricky thing because you don't want me people to get the impression that, oh, like being suicidal is awesome or being so manic you can't sleep for days or you spend all your money in one day is good. It's not. But that, does that necessarily make bipolar mania and depression bad in of themselves? Krista: Well, I think my personal perspective as a person who has been given that label - this is my life that I get live in. I get to make whatever choices stupid or brilliant that I want to make with that one life that I get to live. And there have been times where, what other people, I kind of said this already, but where other people may have looked at my life and thought, she's definitely manic right now. And a lot of those choices I made in that time are choices that have shaped me, that have grown me, that may not have looked like smart choices. So, you know, it's terrible when someone is so manic that they're making choices in their life that are deeply harmful to their being. And that's where it gets complicated around forced treatment and things like that because everybody's on the outside watching is like, this is wrong. You know, they don't even know what they're doing. Right. And everybody is scared and, and it gets, it gets complicated. This is, this is why it's such a touchy, forced, forced treatment is such a touchy issue because does that person have the right to make their own personal choices for their own one life that they get to live from their heart or are they mentally ill and, and they don't know what they're doing. So we better save them because they're going to die or they're going to hurt someone or, right. It's, it's not. So that sometimes the psychiatric survivor movement, um, is, I find it frustrating sometimes because a lot of people in the movement have been really hurt by treatment in a way that I was, I mean, I was hurt by forced treatment, but not some people that have been hurt very deeply and for many years. And, um, and I think that lived experience in a way makes them sort of issue the entire psychiatric model of care as it's bad for everyone. Um, and I don't, and I, I think I used to be like, felt that way a little bit at first when I first started working in the field. But, um, but yeah, I just see things as so much more complicated and nuanced now than I ever did before. You know, when I first started working as an advocate in the mad pride movement, um, I didn't really, I knew a lot less. I knew my personal experience pissed me off, you know, and that's why I started working in the mad pride movement. That's why I started studying recovery. That's why I wanted to educate families about recovery. Um, and now, you know, almost 20 years later, um, I've seen a lot, I've learned a lot and I'm a little more centrist around this stuff. Like I've seen medication help people massively. I've seen families that are utterly torn apart and when the kid gets some meds, they can actually talk again. So it's, I don't, I don't know. I think I departed from your original question, but - Rudy: No, no, that's fine because you opened up a new well. So you talked about forced treatment and I, I've been a victim of forced treatment as well. It's kind of why the show was called No Restraints. I've been put in restraints several times. And something that I always really want to stand for is advocating against forest treatment because I don't think it works. I think it does more harm than good. Yeah. But I talked to a lot of people, pretty much everyone that I talked to you except for maybe one or two that I've interviewed over the past few years, is that there are certain allowances for treatment. What say you to that? Krista: I believe also there are certain allowances and I'm not some, you know, expert on exactly how we should implement that. So like, you know, I don't claim to know exactly under what circumstances specifically written in, codified in law that we should, I mean, it's so hard to (inaudible), you can't play God right? This is what's so like how do we create a system that for the most part, almost never forces people into treatment because I agree with you. I don't think forcing people into treatment works. Um, but then there are some instances, I mean, I know some people who've been really grateful that they've been forced into treatment. I know some people that think that they're grateful only because they'd been indoctrinated by the psychiatric community. I mean, it's just, you know, I feel like the older I get, the less I know, really as unsatisfying as that is. That's kind of what I'm left with. Rudy: No, and that's fine. And I mean, me personally, my views on pretty much everything have gone up and down throughout my entire life. And it's very, very hard to say key issues where if that's the hill that you're going to die on, right? Because most likely 10 20 years from now you're thinking like totally different anyway. But I think always I want to stand for human rights and making sure that people have decisions no matter how sick people say they are and that they're totally incapable. People should always have options. Even if it's just simple things like you, what do you, what do you want to eat? What do you want to drink? Do you want to sit up? Do you want to sit down and write? That goes a long way. Krista: Well, and from a system perspective, again bringing up Patricia Deegan, like I love her work around personal advanced directives. Like that's one way that the mental health system can try at least to make sure that people's choices are being respected to such a degree that ultimately maybe they'll never need to have forced treatment because they've got personal advanced directives in place. So, you know, somebody's personal advanced directive might look like, you know, it's similar to like a wellness and recovery action plan. It might look like these behaviors from me, if I start doing x, Y, Z. If I say start saying these words here's what I want you to do. And most people aren't gonna say, send me to hospital. They're going to say, you know, specific things that resonate for them. Like for some people it would be like, you know, take me to a music concert of my favorite musician to, you know, like people, this is a thing that I think the mental health system does really wrong is we do not incorporate art, poetry and meaning making into treatment enough. And for me, for sure, those are the things like spirituality, art, poetry and meaning making, those are the things that heal me, you know? And I know I'm not alone in that. So, yeah. But there are things we can implement in the system. Like, you know, more peer respite programs. Like alternatives to hospitals so that people don't have to, if they're in crisis, they can get support without, you know, people go to the hospital sometimes just cause they're so desperate. Right. But if there are peer support, res - peer respite houses that offer peer support, that might reduce the need for the, you know, for these cases that evolve into, or it feels like the only option is forced treatment. So I really just think there are a lot of preventative things that as a system we need to be implementing. Rudy: I agree. And you know there's a lot of people in the Treatment Advocacy Center camp who say all these things like art, poetry, pet therapy, this is not going to help the "seriously mentally ill". We need new meds, new treatments. We need Advanced Outpatient Treatment, involuntary care, more beds. That's what's really going to help the "most seriously mentally ill," which is the people that we should be as a society, the government, should be funding should be taken care of. And everyone else, the quote unquote worried well should just get nothing basically or very little or be last in line. What, say you to that? Krista: I don't even know what to say to that. I think the hopeless, the pervasive hopelessness that workers sometimes feel is contagious. And I get it that some people are really, really disabled by their emotional distress to such a degree that functioning were functioning in the world becomes challenging. And I'm not suggesting that, you know, we just create poetry classes for the, for the mentally ill and they'll get better. It's not, it's not like that. I mean people need different levels of care and different levels of care, you know, need to be like, I believe that somebody that like let's say somebody who people think needs forced treatment. The sickest of the sick, the most unwell of the most unwell. That person may need a ton of support, a ton of support, and for a long period of time and the way in which they get that support for a long period of time, I don't think that putting them in a care facility where they're just given meds and it's a hospital like environment and they're not exposed to art, poetry, community, social inclusion and things like that are going to help either. Like, you know, you can't put a seed in soil like that and expect it to bloom. So I don't really know. I don't know. I mean, I'd like to see long longterm programming and residential care for people that need a high level of care for longer periods that also incorporates their humanity in a greater way rather than just reducing their symptoms to a biological brain disease and viewing them sort of divorced from their spirit and humanity and connection to the community outside of the hospital world and outside of their role as a mental patient. Rudy: Now about that word "brain disease," like do you, what do you think of that? You seem to say it with derision, is there nothing going on in the brain? Is it not a disease? Krista: Well, there are, I mean there are things going on in the brain. There's always chemistry in our bodies and in our brains happening. I mean we get excited, our heart beats like there's - you know - there's, there are physiological responses happening to emotions all the time. So of course there's brain activity, but I've yet to see, you know, biochemical markers for mental illness. You know, when people die who have diagnoses of mental illnesses it doesn't show up on brains. It doesn't show up on brain scans in the same way. Or for those who would argue, "well, look at this study." You look at this brain. Those are brains that have also been taking psychiatric drugs for a long time often. So it's hard to tell. It's just not - I don't believe it's a brain disease in the way in an isolated way. I believe the brain is of course, you know, the brain is affected by physiology and by our emotions. And by our thinking. And and all of that. But I don't believe it's a stagnant thing that, you know, that brain is diseased and it's gonna stay diseased for the rest of its life as a human, as this human. No, I don't believe that. Rudy: Well, the National Institute of Mental Health, they need to spend another $10 billion, then they'll find those biomarkers. So we'll get there. Krista: Yeah. Yeah. I know they keep investing money searching for those biomarkers. So... Rudy: Yeah, let's get to Families Healing Together because I was first exposed to NAMI's Family to Family, which sounds a lot different from what you got going on there. Is this a response to that? Like how did you feel compelled, like this was something that was very necessary for you to create? Krista: Yes. So I encourage families to take NAMI's Family to Family as well. So here's the thing, it's like I created Families Healing Together because I was in a position at a drop-in center where my role was to create family supports and to create a curriculum to support families that had people that were struggling with mental health issues, often people who are diagnosed with mental illnesses. And I was googling and trying to find information and all I could find was sort of the medical perspective on what is mental illness. So the commonly agreed upon ideas of illness and disease. And I didn't that that information is so readily accessible. It's all over. It's everywhere. NAMI gives it out, hospitals give it out. It's just everywhere. It's easily, readily accessible. And I think it's important for families to read that, to learn it, to decide what they believe, to be really educated about the choices that they make in their family, about how they want to treat, um, mental health issues. Uh, but what I wanted to do was I wanted to compile in one place different information. And this is when the mental health recovery movement was really starting to blossom. So there were all these new, you know, there were people, psychologists, and lawyers and activists and people tree generating all of this knowledge and sort of like a knowledge community around recovery in this concept that people can get well and stay well and live well. This was blossoming. And so I wanted to harness that and put it all in one place so that it would be easy for families to, to get that perspective too, because it's not the perspective that they get when they just Google, you know, it's not the perspective the hospital gives them. Um, and so, so I, you know, I didn't want to reinvent the wheel and I searched everywhere and couldn't find any kind of curriculum, like what I was hoping to create until I found this tiny little mighty mouse program in Toronto that was doing this work. And, uh, so I joined forces with them and we wrote curriculum and developed at, at family outreach in response program in Toronto. We developed this mental family mental health curriculum. So we developed a 10 week course and an eight week course and we were doing these groups in person with families. (phone alert goes off) I don't know how to shut that damn thing off. I tried twice. I don't know how to stop it. Rudy: You gotta put it on channel three. Krista: What, channel three? (laughs) I don't know. But anyways, yeah, so I was running those groups in person and I was really grateful to the family outreach and response program cause they had developed this amazing curriculum that I got to train with them and learn from. And then I started writing curriculum as well. And then eventually I ended up taking all of that. Krista: People were very interested worldwide in this curriculum because there was nothing else like it. Um, and so I was able to put it online so that it could be more accessible to more people. And it's been online for the past seven years and it's now in the format that it's in online. It's an eight week, it's an eight week, um, online program where people can run the, you know, take it as a group and they communicate with each other in the comments section about the curriculum. Yeah. And they can just sort of explore different ways of understanding what's happening. You know? Rudy: Yeah. I think the first time I think that you reached out to me was wanting to take this course and get my thoughts on that. Why specifically me? Why was I the Chosen One? Krista: I forget how I initially found you, but I remember seeing that you were involved in some organizing around anti-forced treatment, but that you were also working with the National Alliance with Mentally Ill. So I was like, this guy's perfect for, I'd like love to know his opinion on this class because that just seemed like the perfect combination for me cause I saw it and I was like, okay, obviously he's a critic, a critical thinker or he wouldn't be involved in both. Like you're like a knowledge seeker, you know? Um, yeah. And so I was like, I'm just curious. Yeah, but you never gave me your thoughts. Rudy: Yeah. Well, let me, let me, let me tell you this. Krista: (laughs) I would like to interview you. What are your thoughts on the class? Rudy: No, the thing is is that it's a lot. I'm just going to say that there's a lot to follow up. I'm, I'm bad with homework. I'm bad with assignments. I've tried taking online classes before. I always fail, so just because I wasn't able to get through all the classes and all the assignments and everything. Something that I have noticed that I like is that first off, I do not like NAMI's Family to Family. I've sat in on meetings, I've spoken to groups. A lot of times these people, these parents, and you might've gotten these questions or comments from parents that you've worked with is "how do I get my son or daughter sectioned? How do I get them 5150'd, Baker Act, all this stuff. Like how do I get them to take their meds? I'm so sick of them. I'm going to throw them out. Like, I'm just so frustrated." And it always comes from that perspective. And that's not necessarily, I mean for what I've seen, I'm sure all groups are different. All moderators are different. It doesn't come from a place of healing. It just comes from a place of just frustration and just wanting, wanting to be told that they're right, that they're not part of the problem. Krista: Sure, sure. I mean the reason that I like the Families Healing Together curriculum and the reason why I liked running the groups in person in Toronto was because my experience when I would go, I would go to network, you know, with these other family programs that were running support groups in my experience was that the groups were very depressing. They were depressing. They were laden with frustration and angst and the moderators would often just hold space which is an important thing to do. But I think, I think if you want to create an environment in your family where recovery is likely to flourish, you have to be in contact with your own sense of hope. And I don't think that a lot of those groups foster that sense of hope. And so what I find for myself when I'm running family support groups even still, and I'm just starting to run one in person again, that I'm so excited about on Thursdays in the South Bay, in the San Francisco area, is I want families to understand completely that people get well. (inaudible) Like no matter what any doctor says about that your person that you love, they can absolutely get better. They can live a life of meaning, purpose and value, and that you can be connected to them and set boundaries at the same time. So like, let's say you are frustrated and you need to, you want to have them sectioned as you said or whatever. I'm like, okay, well what, what you really want is you want to set boundaries. You want to, you want to know, you want to establish what is okay for you and what is not okay for you and your personal relationship with them. You know, what they do with their life. This is their decision. Um, so let's talk about that. Like what are the boundaries that you need to set and how can you be okay in your relationship with them and stay connected to them and continue to offer unconditional love and presence for them, but maintain your boundaries and you know, that's a whole, that's a whole different way of understanding the relationship. Then I need to get them in the hospital. You know, they're, they're making me crazy in my house. They're not doing the dishes. They're writing on the walls. You know, the, just because you don't, sometimes the answer is that some space needs to be created between in, within the relationship and it's not, that doesn't mean that person has to be forced into treatment. You know, some, some family changes to the entrenched patterns might be enough to, to change that person's behaviors that are appearing to make them seem completely crazy. Rudy: Yeah. That was one of the main things I liked about your training is that it's not about here's these list of diagnoses, here's these symptoms and here's how to basically coerce your son or daughter your loved one. Here's how to lead them down a path. Here's how to navigate the legal system to get what you want. Here's how to bypass certain HIPAA protections. All these, these stuff that I, that I, he me only disagree with. Whereas you are more about options, choices and see, the thing is Krista, is that I'm estranged from my family. I don't talk to them anymore at all. And it was one of the best personal decisions I've ever made for myself. It was for my own good. So it's hard for me to sometimes get into back into that field of mine is that families are great for most people. They are, are oftentimes the strongest thing that someone has in their life as far as compassion for support, for making sure that the person feels safe. And just because I don't have that in my life doesn't mean that it's necessarily bad. I don't know if you get emails or whatever from people saying like, "oh, the families need to stay out of that. Like I hate families. Like why do you want to control everything? Why do you always want to control the conversation?" So I just like that you are so much more beyond that. Krista: Sure. Well, and you know, I've worked with families that haven't been in touch with their relative in many years because of the forced treatment created such a rupture in the family that now the relative no longer speaks to their, their family member. And that's really interesting. That's really interesting work to do with, with people. And, and it's also really interesting work. When people come and they're like, they're so controlling of their family member and it comes from a place of love and fear and all of that, but they're there. So they're family members. Distress has completely become their life. And it's really interesting untangling that with people and helping them to realize that their relationship can actually be really beautiful and strong when they back away a little. And when they allow for more personal choice and freedom and when they create systems and structures in the family home that give more autonomy to the, the person who's got the label or who's got the, you know, the identified patient in the family. And that's really beautiful work in it. And my concern about, you know, nanny is interesting cause some chapters are really great, some are like, you know, they're an organization and every chapter is different and all of that. But some of the groups that I've been to, I feel like foster a continuing of learned helplessness, you know. Yeah. And so a lot of the work that I've done with Families Healing Together is to try and help all the members in the family to find their personal sense of freedom. Um, and that includes the person in recovery. And that includes, you know, the mom, the dad, the brother, the sister that feel, that feel, you know, it's like all of the voices are important and need to be heard and need to be out in the open and valued and structures and systems can be put in place in a family where everybody's autonomy is respected, even in extreme mental health distress. Uh, but they need support to do that. I mean this medications are so fascinating and families because the hospital tells the family it's their job to keep the relative on the medications. Oftentimes, you know, they're discharged, they go back home and the hospital is like, you got to make sure that your relative stays on their meds. That's a recipe for creating a family dynamic that's not healthy. Rudy: Yeah. And all that you said. The good things that - the last part - is really why I think Families Healing Together is very necessary. And if one person watching this and signs up for one of your programs, like mission accomplished because I really think more and more people should know about it because it is much needed in our society. Krista: Yeah. Thank you. I've been doing Families Healing Together full-time for seven years and it last October I started working at jobs and I got a full time job and so I'm Canadian. I lived in Canada, I moved to Costa Rica, lived there for about four years and then I moved to California. I've lived here since 2015 and in October I got a job, my first job in the United States at a national behavioral Healthcare Corporation, publicly traded a big corporation, uh, that does addiction rehab facilities. And it was like such a culture shock to me. And I began to see firsthand just how the American insurance industry works and how the addictions addiction field works with all the, it's so competitive for to get people into the treatment facilities and it's like, it's just drenched in capitalism in this way that's so jarring to me. And so I had to leave that kind of environment. Working in that kind of environment wasn't, wasn't for me. And I found a small facility. It's a 22 bed facility that's local to where I live that I've just like, I've just fallen. So in love with this facility, it's, it's small. It's 22 beds. We serve boys age 12 to 17 with substance use and mental health issues. So there's both, you know, people with substance use and no diagnoses of mental health issues. There's people that have diagnoses and they don't have substance use. There's both but sort of like a wide cross section of kids, boys age 12 to 17. And I love our psychiatrist. I think he has really good work with the boys and it's just nice to, it's nice to have found. I've been working for so long with families around kinda like framing their experience and talking about their feelings and learning to set boundaries and now I'm doing this, this sorta like this other kind of work where I still get to do that in the community because the organization that I worked for, Muir Wood allows me to be a support to the community in that way. And then I also get to, you know, try and bring kids that need that kind of treatment to a place where they'll get good treatment. Cause you know, that was me. I mean, I wasn't a boy, but I was a 16 year old kid that was having some, some emotional distress. I didn't think it was distressed at the time, but, and it was largely related to drug use, I think. Or maybe not. I don't know. I had sexual trauma, I was little. Maybe it was that. But like I see these kids that we serve at Merewood where I work and they're like, you know, they just, they, they get good treatment. They get, they get equine therapy, they get, it's like personal development boot camp. I mean when I was in the hosp - I was forced into treatment that there was nothing, there was no talk about. Krista: It was really, you know, not that. So anyway, I'm really, I feel really blessed to work in a place where, you know, they get fed really good food, they go surfing and they do adventure therapy. They do equine with the horses. I know they have groups all day, they do different groups. They're in school still so they don't lose their credits, which is like, that's a big, big part of when you're young and you get forced into treatment and then you like lose a semester. I mean, like that doesn't happen with the boys that come to Muir Wood, so anyways, I'm still doing Families Healing Together, but not as much anymore. Like, I kind of have, my heart has found a home with this facility that I'm working with now. I love, I'm still helping families and Muir Wood graciously sponsors me to continue to do that, so anyone can call me and I'll help connect them to treatment and work with them. Rudy: They're lucky to have you. Last topic before we bring it home, how was your family situation like, do you ever struggle to say, take your own lessons that you teach and apply them into your own family situation? Krista: Yeah, like from a cosmic perspective, I think that, uh, I think that I created Families Healing Together for myself because I would need it when my teenagers became teenagers. So I haven't - I have an 18 year old and he was born in 2000. His birthday's in September, and then I have one turning 14 in July and a seven year old. And yeah, everything in Families Healing Together is all of that curriculum is lessons that I need super big time with my own kids. And I don't think I'm a perfect mom by any means or even a great mom. I think I'm mom. Okay. Mom. And I'm grateful that I have access to, you know, and that I have interest in studying and practicing things to help me be a better mom. And a lot of that is stuff that's, you know, in the Families Healing Together, recovering our families class. Yeah. Rudy: Now, are your, are your older kids ever like, "don't try that Families Healing Together bullshit on me!" Krista: No, I don't think so. I mean, I don't know. Rudy: No, I mean, but Krista: So people though, like people that take the class will be like, "you know, I tried this with my relative and they were like, what, what are you doing? Like, you don't sound like yourself." So like this happened, but, I mean, I don't know. Not, I don't think my kids sometimes, I mean, you know how like if you're like a conservative, you'll raise a hippy? So that, that kind of has happened in my family in some ways. Um, but, but yeah, I don't know. That's personal stuff, I guess. Rudy: Yeah, no, it is what it is. And something, something that I've heard time and time again, especially when I interview parents, is that you can be the best parent. You can be - everything by the book and just be a model parent and do all the lessons and everything. But if your kid's an asshole, like there's only so much you can do. Krista: Well, I mean, if your kid's an asshole, there's probably a reason they're being an ass. Yeah, totally. Yeah, but this is, but it's, I mean, relationships are hard, so hard, just friends, relationships with friends are hard. Relationships with romantic partners are hard. And then parental child relationships, that's a whole other level of hard. It's really hard, you know? I mean, it's like all of your stuff is triggered as a child in the family dynamic. All your stuff is triggered by your parents. And when you become a parent, you know, it's like you're getting it from all these layers because you're seeing yourself act in ways you don't want to act. And then you're mad at yourself for acting that way and then your kid is triggering you because you're like, you know that that reflects poorly on me or whatever. I mean it's just like it's a minefield parenting is a minefield. It's really work. Rudy: Yeah. I heard from one parent who's anti-forced treatment said, "you know what, sometimes my kid just makes me so mad. I just want to force the meds down their throat." So just, okay. Krista: Yeah. Uh, I mean, yeah. So, so I'd meet with that parent. Like if I were working with that parent, I would spend a lot of time with that parent talking about their anger because that's, that's unexpressed, you know, my suspicion is that probably their, um, you know, they've just come to a point of complete exhaustion. And so well, you know, how can they in the future not let themselves get to that place of complete exhaustion. So like what are all the things that they've allowed to happen by not sending from boundaries that have got, that have had them land at that place where they're like, cause there's this, there's this family involvement continuum that I like to talk about. That goes from neglect to overprotect. And I see families wildly swinging from this neglect overprotect. So they'll do the overprotecting where they try and control everything. They try and arrange all the outcomes. They try and set them up with volunteer work and community service and, and all these things that are good for them because they know what's best for their relatives. And of course the relative rails against all of that because they have their own ideas and then they swing. Then the a big fight will erupt and then the parent will swing back to neglect, which is I'm just going to shove the meds down their throat. Right. Like in that case example that you use. But neglect looks like all sorts of different things, you know. And like neglect sometimes looks like forcing someone to treatment because they can't deal with it anymore. Not, because like sometimes it's not happening for the right reasons. It's like, you know, yeah. Right. So, yeah. Rudy: You know, you know, Krista, if I ever have kids, which is not gonna be any time soon, um, I'm definitely going to have to take one of your classes because I'm, like I've said before, I can't say enough good things about it. I'm glad that you invited me into the program that you reached out, you took that risk and that you took the risk by coming onto No Restraints. Even though like we're not on Facebook Live and you thought we were only gonna talk for like 20 minutes and look at it's, we're, we're about to hit the 50 minute mark. So, okay. Like I always say, it's always the shy people who end up talking the longest and having the most fun. All right, so thank you. I'm going to let you have the final words, um, even though I'm going to talk after you or whatever. Sure. Yeah. Anything you want to promote, any links, I'll make sure to leave the links to the stuff we talked about down in the comments below so people can check it out and can stay updated. I know you have like a contact form on there, so when you do your next online course, I hope people can check it out. Krista: Yeah, I mean I, and then if you are living in the Menlo Park, San Jose area, uh, I'm running a support group on Thursday nights. So call me (415) 335-9783. Call me and tell you about that. Rudy: Do not call this number for any other reason. (laughs) Krista: No, whatever. It's fine. Call me. Yeah, I'm, uh, I'm just starting this support group and I haven't done one in person in a long time. I'm really excited and I've been, I've been, I have the space but people don't know about it yet. So it's, it's quiet. So if you come you, you know, it might be just a very small, intimate, sweet groups. So, and the point of the group is just to get support for yourself. If you're somebody that loves someone struggling with mental health and addiction issues and I can help. Rudy: And I might, I might just show up randomly. You never know, so... Krista: That's cool. That'd be cool. Yeah. But I really want to be able to connect families to services that I think are, that are good services, good treatment programs and um, and I want to support families to connect with each other because they're their own, you know, when they can build peer support, that's really powerful. So any, I want to be a channel for supporting that Rudy: And the website is FamiliesHealingTogether.com. Krista: Yeah. And MuirWoodTeen.com. Rudy: Cool. I will definitely leave that below. How can people follow you on Snapchat? Krista: So I don't know. (laughs) Rudy: Just kidding. I'm just kidding. Krista: All right. Rudy: Okay. All right. Krista: Snapchat. Should I be on Snapchat? Rudy: Every once in they come out with a cool face filter. So by all means, knock - you'll, you'll, you'll be more popular with your younger kids. How about that? Krista: Thanks. Great. Rudy: Okay. Thank you so much. Thank you for rolling with the punches. Hopefully the great Facebook Outage of Today is gone soon. So I can upload this because it's great content and it deserves people's awareness and hopefully it when you watching this, whatever it is today, tomorrow, this year, um, please leave comments, um, and make sure to still ask questions. I'll make sure that Krista can get to them when she can within the midst of her busy, busy schedule. So that's this week's show. I'll be back next week and the week after that for No Restraints with Rudy Caseres. Thank you, Krista McKinnon. I'll see you all next week. Because it's for your own good.
0 Comments
Leave a Reply. |
Details
ABOUT RUDY
|